Independent Medical Examinations (IMEs) play a pivotal role in the assessment of individuals grappling with dementia and cognitive impairments.
When concerns arise regarding a person’s cognitive function, qualified neurologists or neuropsychologists often conduct IMEs, providing invaluable insights.
During these examinations, a battery of cognitive tests and assessments is administered to objectively evaluate memory, reasoning, attention, and various other cognitive functions.
In addition, a comprehensive review of the patient’s medical history, imaging studies, and neurological examinations is carried out.
The findings from these IMEs not only aid in diagnosing the type and severity of dementia but also assist in tracking the progression of the disease and tailoring treatment plans.
IMEs in dementia and cognitive evaluation are crucial not only for medical diagnoses but also for legal and insurance purposes, ensuring individuals receive the necessary care and support.
Using IMEs for Dementia & Cognitive Evaluation
Independent Medical Examinations (IMEs) play a crucial role in the assessment of individuals with dementia and cognitive impairments.
In cases where there are concerns about a person’s cognitive function, an IME conducted by a qualified neurologist or neuropsychologist can provide valuable insights. During the IME, various cognitive tests and assessments are administered to objectively evaluate memory, reasoning, attention, and other cognitive functions.
A comprehensive review of the patient’s medical history, imaging studies, and neurological examinations is conducted. The results of the IME can aid in diagnosing the type and severity of dementia, tracking disease progression, and informing treatment plans. IMEs in dementia and cognitive evaluation are instrumental not only for medical diagnosis but also for legal and insurance purposes, helping to ensure that individuals receive appropriate care and support.
What is the cognitive ability test for dementia?
The cognitive ability test for dementia is a diagnostic tool used to assess an individual’s cognitive functioning and determine the presence or severity of dementia.
This test evaluates various domains of cognitive abilities, including memory, attention, language, and problem-solving skills. It may involve a series of questions, puzzles, or tasks that assess different aspects of cognitive functioning.
The results of the cognitive ability test can help healthcare professionals in diagnosing dementia and planning appropriate treatment and support for individuals with cognitive impairments.
Can cognitive stimulation benefit people with dementia?
Cognitive stimulation refers to activities and exercises that are designed to engage and challenge the cognitive abilities of individuals with dementia. These activities aim to stimulate thinking, memory, attention, and problem-solving skills in order to preserve and potentially improve cognitive functioning.
Numerous studies have shown that cognitive stimulation can indeed benefit people with dementia. Engaging in cognitive stimulation activities has been found to improve cognitive function, overall well-being, and quality of life for individuals with dementia. It can also help to slow down the decline in cognitive abilities and delay the progression of the disease.
Cognitive stimulation activities can take various forms, including puzzles, games, reminiscence therapy, art therapy, music therapy, and group discussions. The activities are typically tailored to the individual’s abilities and interests, and are often conducted in a supportive and social environment.
In addition to the positive effects on cognitive function, cognitive stimulation can also provide emotional and social benefits for individuals with dementia. It can help to reduce feelings of isolation, promote social interaction, boost self-confidence, and enhance mood.
It is important to note that cognitive stimulation is most effective when it is provided on a regular and consistent basis. It is recommended that individuals with dementia engage in cognitive stimulation activities for at least 30 minutes a day, several times a week.
However, it is important to consult with a healthcare professional or specialist when implementing cognitive stimulation activities for individuals with dementia. They can provide guidance on suitable activities, the appropriate level of challenge, and any modifications that may be necessary based on the individual’s specific needs and abilities.
Overall, cognitive stimulation offers a non-pharmacological approach to managing and improving cognitive impairment in individuals with dementia. It has the potential to enhance cognitive functioning, emotional well-being, and overall quality of life for individuals living with this condition.
What stage of dementia is associated with severe cognitive impairment?
In the evaluation of dementia and cognitive disorders through independent medical examinations (IMEs), it is important to understand the different stages of dementia and the associated levels of cognitive impairment. One stage of dementia that is particularly associated with severe cognitive impairment is the advanced or late stage of the condition.
In this stage, individuals with dementia often experience significant memory loss and may struggle with basic daily activities, such as dressing, toileting, and eating. They may also experience difficulties with language and communication, have difficulty recognizing familiar faces or places, and exhibit changes in behavior and personality.
At this stage, individuals may require extensive assistance and supervision to ensure their safety and well-being. They may have difficulty following instructions, exhibit confusion, and experience problems with problem-solving and decision-making. In some cases, individuals may become completely dependent on others for their care.
It is important for medical professionals conducting IMEs for individuals with dementia to be aware of the stage of the disease in order to accurately evaluate the cognitive impairment and its impact on the individual’s daily functioning and overall quality of life. The assessment may include observations of the individual’s behavior and interactions, as well as cognitive testing and interviews with both the individual and their caregivers.
Understanding the stage of dementia associated with severe cognitive impairment can help guide the recommendations and interventions provided through the IME process. This could include identifying appropriate support services, recommending modifications to the individual’s environment to enhance safety and comfort, and providing resources and strategies to support the individual and their caregivers in managing the challenges associated with severe cognitive impairment.
What are the 4 levels of cognitive impairment?
In the evaluation of cognitive disorders, such as dementia, there are generally four levels of cognitive impairment that are recognized. These levels are used to gauge the severity of cognitive decline and assist in determining appropriate treatment and intervention strategies. The four levels of cognitive impairment are as follows:
1. Mild cognitive impairment (MCI): This is the mildest form of cognitive impairment and typically involves a noticeable decline in cognitive function that is beyond what is considered normal aging. Individuals with MCI may experience memory problems, difficulties with language and communication, and challenges with executive functioning. While individuals with MCI may still be able to perform their daily activities independently, they may require extra support and monitoring.
2. Moderate cognitive impairment: At this stage, individuals may experience more pronounced memory loss and cognitive difficulties. They may have difficulties with problem-solving, decision-making, and may struggle with complex tasks. In addition, individuals at this stage may also experience behavioral and personality changes, and require significant assistance with daily activities.
3. Severe cognitive impairment: At this stage, individuals with dementia experience a significant decline in cognitive function, including memory loss and difficulty with language and communication. They may require constant supervision and assistance for daily activities and may have difficulty recognizing familiar people and places. Behavioral symptoms, such as agitation and aggression, may also be present.
4. Profound cognitive impairment: This is the most severe level of cognitive impairment, where individuals with dementia experience a complete loss of cognitive function. They may be unable to communicate, recognize loved ones, or carry out basic activities of daily living without assistance. Individuals at this stage require 24-hour care and support.
It is important to note that the progression and severity of cognitive impairment can vary from person to person, and there may be overlap between the stages. Additionally, the terms and categorizations used to describe the levels of cognitive impairment may vary in different sources and healthcare settings.
The Progression of Mild Cognitive Impairment
Mild cognitive impairment (MCI) is a condition that involves a noticeable decline in cognitive abilities, but it is not severe enough to be classified as dementia. It is important to understand the progression of MCI, as it can provide valuable insights into the potential development of dementia in individuals.
The speed at which mild cognitive impairment progresses can vary from person to person. In general, MCI tends to progress slowly over time, but the rate of progression can be influenced by various factors, such as age, overall health, and underlying causes of cognitive impairment.
Studies have shown that approximately 10-20% of individuals with MCI progress to develop dementia each year, while others may remain stable or even experience improvements in their cognitive functioning. It is estimated that about 80% of individuals with MCI will eventually develop some form of dementia within 6-12 years.
It is worth noting that not all cases of MCI will progress to dementia, and some individuals may live with MCI without experiencing a significant decline in cognitive abilities. However, it is important for individuals diagnosed with MCI and their caregivers to be aware of the potential risks and to regularly monitor cognitive functioning.
Early detection and intervention are crucial in managing MCI and potentially slowing down its progression. Individuals diagnosed with MCI can benefit from various interventions, including cognitive stimulation activities, regular exercise, social engagement, and a healthy lifestyle. These interventions can help maintain cognitive function and potentially delay the onset of dementia.
Overall, understanding the progression of mild cognitive impairment is essential in providing appropriate care and support for individuals at risk of developing dementia. Regular assessments and monitoring of cognitive abilities, along with the implementation of appropriate interventions, can contribute to a better quality of life for individuals living with MCI.
Mild cognitive impairment vs dementia
Mild cognitive impairment (MCI) and dementia are both conditions that affect cognitive functioning, but they differ in terms of severity and overall impact on daily functioning.
Mild cognitive impairment is considered to be a transitional stage between the normal cognitive decline of aging and the more severe cognitive impairment associated with dementia. People with MCI experience a noticeable decline in cognitive abilities, such as memory, language, attention, and problem-solving skills, but they are still able to carry out their daily activities independently. This condition does not significantly interfere with their overall functioning.
On the other hand, dementia is a more advanced and progressive condition characterized by a significant decline in cognitive abilities, including memory loss, impaired judgment, confusion, and changes in behavior and personality. Dementia affects a person’s ability to perform daily activities and often requires assistance or supervision.
One key difference between MCI and dementia is the level of impairment and the impact on daily life. Individuals with MCI may be aware of their cognitive decline and may experience frustration or concerns about their memory loss, but they can generally manage their daily activities with some compensatory strategies. In contrast, dementia severely impairs a person’s ability to independently perform daily tasks and affects their overall quality of life.
Another difference is the progression of the condition. Mild cognitive impairment can remain stable over time, with some individuals even recovering their cognitive abilities, while others may progress to dementia. Dementia, on the other hand, is a progressive condition with symptoms worsening over time.
It is crucial to differentiate between MCI and dementia as they require different management strategies and interventions. Early detection and proper diagnosis by healthcare professionals specializing in cognitive disorders, such as through independent medical examinations (IME), can play a crucial role in identifying the condition accurately and providing appropriate support and care.
Conclusion
The use of Independent Medical Examinations (IMEs) in the evaluation of dementia and cognitive impairments represents a vital component of comprehensive healthcare assessment.
IMEs offer an objective and expert-driven approach to understanding the cognitive health of individuals, helping to diagnose dementia, assess its severity, and inform tailored treatment plans. These examinations bridge the gap between medical diagnosis and legal or insurance considerations, ensuring that individuals receive the appropriate support and care they need.
As our understanding of dementia and cognitive disorders continues to evolve, the role of IMEs becomes increasingly significant in providing accurate diagnoses, tracking disease progression, and enhancing the overall quality of life for those affected.
By relying on the expertise of neurologists and neuropsychologists in conducting IMEs, we can empower individuals and their caregivers with the knowledge and resources necessary to navigate the challenges posed by cognitive impairment and dementia.
Further Considerations
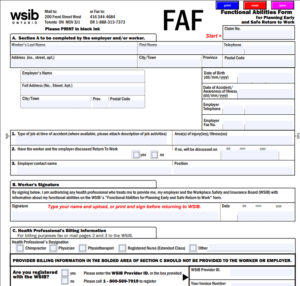
1. Difficulty in obtaining accurate medical history: When conducting an independent medical examination (IME) for individuals with dementia or cognitive impairments, gathering an accurate medical history can be a challenge. Patients with these conditions may have memory loss or difficulties in communicating their medical history, making it harder for the examiner to obtain a comprehensive understanding of their condition.
2. Assessing cognitive function: Evaluating the cognitive function of individuals with dementia or cognitive impairments can be challenging. The examiner needs to use specialized assessment tools and techniques to measure different aspects of cognitive function accurately. This requires expertise and experience in working with individuals with cognitive disorders.
3. Identifying the cause and subtype of dementia: There are different causes and subtypes of dementia, each requiring different approaches to management and treatment. Determining the cause and subtype of dementia is crucial for providing appropriate care. However, accurately diagnosing the cause and subtype of dementia through an IME can be complex, as it often requires additional specialized assessments and diagnostic tests.
4. Assessing functional impairment: Besides evaluating cognitive function, an IME for individuals with dementia also needs to assess functional impairment in daily activities. This includes activities such as cooking, bathing, dressing, and managing finances. Determining the level of functional impairment accurately can be challenging, as it requires evaluating the individual’s abilities across various domains of daily living.
5. Communicating findings effectively: After conducting an IME for dementia or cognitive impairments, effectively communicating the findings to the relevant parties is crucial. This includes providing clear and concise reports that summarize the assessment results, diagnosis, and recommendations. However, conveying complex information about cognitive disorders in a way that is easily understandable by non-medical professionals can be challenging. It requires skill in presenting information in a clear and accessible manner.
FAQs (Frequently Asked Questions) About Dementia and Cognitive Impairment
1. What is the cognitive ability test for dementia?
– The most commonly used cognitive ability test for dementia is the Mini-Mental State Examination (MMSE). It evaluates various cognitive functions, such as memory, attention, language, and visuospatial skills.
2. Can cognitive stimulation benefit people with dementia?
– Yes, cognitive stimulation activities, such as puzzles, memory games, and music therapy, can help improve cognitive function and overall quality of life for individuals with dementia.
3. What stage of dementia is associated with severe cognitive impairment?
– Severe cognitive impairment is typically seen in the later stages of dementia, such as in advanced Alzheimer’s disease or other forms of advanced dementia.
4. What are the 4 levels of cognitive impairment?
– The four levels of cognitive impairment are: normal cognition, mild cognitive impairment (MCI), moderate cognitive impairment, and severe cognitive impairment or dementia.
5. How fast does mild cognitive impairment progress?
– The rate of progression of mild cognitive impairment (MCI) varies from person to person. Some individuals with MCI may progress to dementia within a few years, while others may experience a very slow decline or even remain stable for an extended period.
6. What is the difference between mild cognitive impairment and dementia?
– Mild cognitive impairment (MCI) refers to a stage of cognitive decline that is greater than expected for a person’s age but does not meet the criteria for dementia. Dementia, on the other hand, involves severe cognitive impairment that significantly interferes with daily functioning.
7. Are there any medications that can slow down cognitive decline in dementia?
– While there is no cure for dementia, certain medications, such as cholinesterase inhibitors and memantine, can help manage symptoms and slow down cognitive decline in some cases.
8. Can lifestyle factors affect the risk of developing dementia?
– Yes, there is growing evidence that certain lifestyle factors, including regular exercise, a healthy diet, social engagement, and cognitive stimulation, may help reduce the risk of developing dementia.
9. Can dementia be prevented?
– While it is not possible to completely prevent dementia, adopting a healthy lifestyle and managing underlying health conditions, such as hypertension and diabetes, may help lower the risk or delay the onset of cognitive decline.
10. Are there any support services available for individuals with dementia and their caregivers?
– Yes, there are numerous support services available for individuals with dementia and their caregivers, including memory clinics, day care programs, support groups, respite care, and home assistance services. These resources can provide valuable guidance, education, and emotional support throughout the journey of dementia.
Glossary of Terms Used in the Article
1. Cognitive ability test: A test designed to evaluate a person’s cognitive functions and abilities, often used to diagnose dementia.
2. Dementia: A general term for a decline in mental ability severe enough to interfere with daily life, often associated with memory loss and impaired thinking.
3. Cognitive stimulation: Activities or interventions that aim to stimulate and maintain cognitive function in individuals with dementia.
4. Stage of dementia: A level or phase of progression in the severity of dementia, often categorized based on the level of cognitive impairment.
5. Severe cognitive impairment: A stage of dementia characterized by a significant decline in cognitive function, including memory, language, and problem-solving abilities.
6. Levels of cognitive impairment: Different stages or levels of decline in cognitive function, ranging from mild to severe.
7. Mild cognitive impairment (MCI): A condition in which individuals experience a noticeable decline in cognitive abilities beyond what is expected for their age, but not severe enough to be diagnosed as dementia.
8. Progression: The rate at which a condition, such as mild cognitive impairment, develops or worsens over time.
9. Diagnosis: The identification or recognition of a particular disease or condition based on symptoms, tests, and medical evaluations.
10. Symptoms: Indications or signs of a disease or condition that are experienced by an individual.
11. Memory loss: The inability to recall or remember information or events accurately.
12. Impaired thinking: Difficulties in reasoning, problem-solving, decision-making, or other cognitive processes.
13. Daily life: Activities and tasks that individuals typically engage in as part of their regular routine and functioning.
14. Mental ability: The overall capacity or capability of an individual to think, reason, perceive, and understand.
15. Interventions: Actions or strategies implemented to address or manage a particular condition or problem.
16. Decline: A gradual decrease or deterioration in the level or quality of something, in this context, referring to cognitive abilities.
17. Function: The ability to perform tasks or activities effectively and efficiently.
18. Evaluation: The assessment or examination of something, often to determine its value, quality, or condition.
19. Language: The system of verbal or written communication used by humans.
20. Problem-solving abilities: The capacity to analyze, evaluate, and find solutions to problems or challenges.